Atlas Systems Named a Representative Vendor in 2025 Gartner® Market Guide for TPRM Technology Solutions → Read More

Fast Provider Onboarding: Reduce Credentialing Delays


8 min read | Last Updated: 27 Jan, 2026
Provider onboarding and credentialing remain two of the most critical and costly processes in healthcare operations. Yet, despite their importance, they’re often slowed by manual workflows, redundant data entry, and complex verification requirements. Every delay has a ripple effect: physicians wait to see patients, revenue cycles stall, and patients experience longer wait times for care.
Credentialing, the backbone of onboarding, demands precision. Healthcare organizations must meet strict National Committee for Quality Assurance (NCQA) standards, including primary source verification, ongoing monitoring, and meticulous reporting. When handled inefficiently, this process not only drives up administrative costs but also risks compliance gaps and physician frustration.
This article explores how healthcare organizations can modernize provider onboarding and credentialing without compromising on compliance or care quality. It also examines how solutions like PRIME® by Atlas Systems are transforming this process through automation, real-time data management, and intelligent verification.
The Importance of Efficient Provider Onboarding
The biggest benefit of efficient provider onboarding is that it ensures new medical professionals are quickly integrated into the system and can start seeing patients. The Bureau of Health Workforce projects a huge physician shortage between 2022 and 2037, and an automated onboarding process reduces the administrative burden, enabling doctors to start seeing patients and offer timely care.
A provider lifecycle management tool like PRIME® by Atlas Systems streamlines the entire process by automating data collection, verification, and compliance checks. It reduces administrative burdens, speeds up provider enrollment, minimizes errors, and ensures providers are credentialed accurately.
Reducing provider onboarding time gives medics a great first impression of your healthcare organization and can be a key selling point to highlight to them. A well-structured healthcare provider onboarding process makes new hires feel valued and supported from day one. This results in higher retention rates and improved patient satisfaction.
What is Provider Onboarding and Credentialing?
Provider onboarding is the process healthcare organizations use to integrate new medical professionals into their system. It includes orientation, training, paperwork, and granting providers access to the necessary resources to begin their work. It involves setting up payroll and IT access and getting trained on organizational policies.
Credentialing is a more regulated process that involves verifying a provider’s qualifications to ensure they meet industry and legal standards for patient care and are competent to practice.
In a nutshell, onboarding is the entire journey of integration, while credentialing is the critical step of verifying a medical professional’s competence and legitimacy before they are granted privileges and enrolled with payers.
Key Steps in the Provider Onboarding Process
This provider onboarding and credentialing checklist will help you understand the provider onboarding process in a healthcare facility:
Step 1: Application
The healthcare provider completes an online application by request or at will and provides all the requested documents. This gives the credentialing team the information they need to verify qualifications and onboard the provider. If any information is missing, the team follows up until all documentation is received. Some facilities use provider onboarding software with alerts, reminders, and calendars to speed up the process.
Step 2: Credentialing
Credentialing involves checking with the issuers of licenses and certificates to verify their authenticity. This is the most critical step in credentialing, typically occurring after a completed application is received. The hiring organization verifies things like DEA registration, medical licenses, NPI numbers, and specialty board certifications. Failure to verify provider credentials, licenses, and board certifications can put healthcare organizations at risk of non-compliance with state and federal regulations, payer requirements, and patient safety standards.
Step 3: Privileging
After the credentialing team verifies that the supporting documents are authentic, it decides the specific clinical privileges to grant the provider. This involves defining the exact procedures and treatments the medical professional can perform within the organization. The provider may be granted full privileges or provisional privileges based on the results of the review process.
Step 4: Enrollment
Once specialty credentialing and privileging are complete, the healthcare facility submits the provider’s documentation to payers to demonstrate their eligibility and qualifications. The documentation must meet payer-specific criteria and comply with billing and reimbursement guidelines. The payer organization then reviews the provider’s compliance with participation criteria and grants or denies approval for enrollment. An approved provider can deliver care to the insurance network’s patients and get reimbursed according to the agreed-upon terms and fee schedules.
Step 5: Ongoing monitoring
Healthcare organizations must perform continuous monitoring and providers’ qualifications and certifications that expire after certain periods, like licenses, DEA status, OIG/GSA exclusion, and malpractice insurance. Automation speeds detection and reduces risk. It’s also important to conduct Ongoing Professional Practice Evaluation (OPPE) to measure outcomes, volumes, complaint trends, and trigger interventions if standards slip.
Step 6: Recredentialing
Periodic re-credentialing to help providers maintain their privileges and comply with current regulatory requirements. Re-credentialing is typically performed every two to three years, depending on the state or accrediting body's regulations and the healthcare facility's specific requirements.
Provider Onboarding Best Practices to Reduce Time & Costs
An efficient provider onboarding process does more than just save time; it smooths out the workflow and ensures a seamless transition from recruitment to active patient care. Here are the best practices for reducing onboarding time.
Have different provider onboarding packets based on specialty
It’s important to create different onboarding packets for each provider type because regulatory requirements, responsibilities, and workflows vary across roles. For example, a physician may need detailed credentialing documents and EHR training, while a locum provider may need specific compliance forms, orientation materials, and role-specific policies. Customizing onboarding packets ensures that providers receive the most relevant information, including resources, training, and documentation tailored to their specific role.
Align start dates with key milestones
In most healthcare organizations, provider start dates are based on when a provider is ready to begin working, rather than payer requirements. If a provider is not yet enrolled with a payer, their services can’t be reimbursed. Identify the payers the provider will be working with, the average turnaround times for enrollments, and prioritize the ones with the highest patient volumes or revenue. This can help you set realistic start dates that align with your organization’s financial and operational goals.
Provide ongoing training and development
Continuous professional development ensures that healthcare providers stay current with industry advancements, enhance their skills, and deliver high-quality services. Provide flexible and accessible training experiences and measure training effectiveness.
Technology Solutions for Streamlined Provider Onboarding
Technology plays a critical role in streamlining the complex provider onboarding process. Advanced technologies like AI and Blockchain are moving beyond simple workflow automation and actively transforming provider onboarding. Here are the tech solutions that streamline the process:
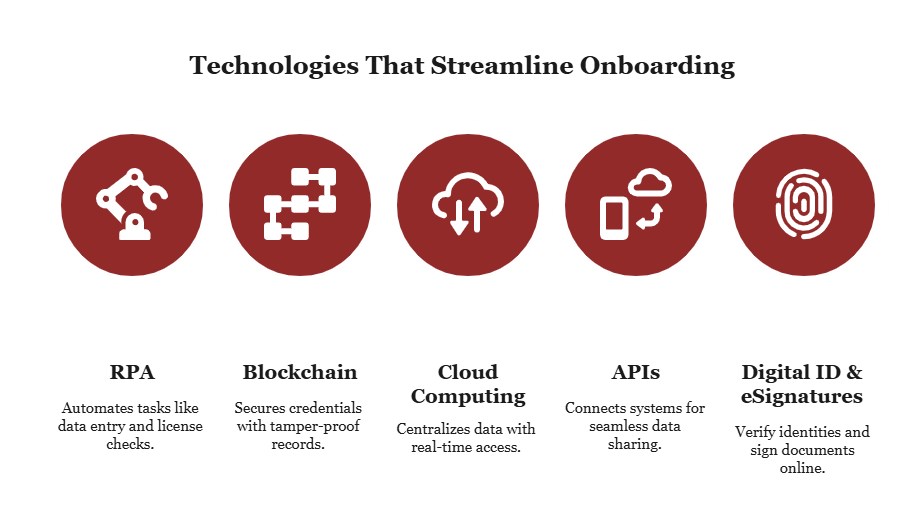
Robotic Process Automation (RPA)
Some healthcare organizations use this technology to streamline repetitive and time-consuming provider onboarding tasks like data entry, license verification, and document routing. They minimize the risk of human error and speed up the onboarding process. When these routine processes are handled automatically, credentialing teams can focus on higher-value activities, such as verifying complex credentials.
Blockchain
A blockchain ledger provides a secure, tamper-proof database for credentialing data that’s accessible to all authorized participants. There’s no need for repeated verification, as each record—whether it’s a medical license, certification, or malpractice history—can be verified without relying on manual confirmation. Provider data can be shared with payers and other healthcare organizations quickly and safely. Blockchain reduces fraud and makes processes transparent for regulators and internal compliance teams.
Cloud computing
Cloud-based healthcare provider onboarding solutions centralize and secure information. They feature real-time updates, enhancing collaboration between new providers and credentialing teams. Providers can submit their documents online, and credentialing officers can track the status of each credential. Documents are never lost, and credentialing workflows stay organized.
Application Programming Interfaces (APIs)
APIs connect credentialing platforms with electronic health records (EHRs), payer databases, and human resources systems. Data flows seamlessly between systems, reducing manual entry and boosting consistency across platforms. Healthcare organizations that use APIs to connect multiple systems can maintain up-to-date provider information and automate routine notifications, such as recredentialing reminders or license expiration alerts.
Digital identity and electronic signatures
These two technologies streamline authentication and approval processes for new providers. Secure digital IDs verify the identities of providers, while electronic eSignatures allow them to complete policy agreements, HIPAA acknowledgments, and other compliance documents online. This speeds up the onboarding timeline and ensures that legal and regulatory requirements are met without delays.
Ensure Compliant, Faster Onboarding with PRIME®
If your provider onboarding process is taking too long and frustrating providers and patients, try PRIME® by Atlas Systems. Our healthcare provider onboarding solution is designed to simplify onboarding. Features like automated credentialing, secure document storage, licensing, and real-time updates streamline the provider onboarding process from day one.
PRIME® has a 95% success rate in accurately verifying and updating provider information through direct outreach. It ensures a faster and more efficient credentialing process by staying up-to-date on current requirements and eliminating unnecessary steps.
Schedule a free demo today and discover how straightforward the credentialing process can be with the right partner.
Provider Onboarding: Frequently Asked Questions
1. How can healthcare organizations reduce provider onboarding time?
Healthcare organizations should have a structured onboarding process and use provider onboarding software to reduce onboarding time. They can also start the credentialing process early to manage expectations regarding the start date.
2. What are the top challenges in provider credentialing?
Some of the top challenges in provider credentialing include lengthy processing times, inconsistent payer requirements, challenges with primary source verification, and a lack of standardization.
3. How does automated onboarding software improve provider efficiency?
Automated onboarding software improves provider efficiency by eliminating manual data entry, digitizing workflows, and automating repetitive tasks like compliance checks and document verification.
4. What metrics should be tracked to measure onboarding success?
Some of the metrics that measure onboarding success include provider retention rates, time to productivity, and compliance rates with training and regulatory requirements.
5. How can onboarding checklists improve compliance and retention?
A provider onboarding and credentialing checklist provides a clear, structured process, ensuring compliance with the company's policies as well as federal and state regulations. Providers avoid many unnecessary steps, start working, and are happier with their jobs.
6. What strategies help lower the cost of provider onboarding?
Strategies that reduce provider onboarding costs include having a standardized process, investing in provider onboarding software, and training credentialing staff.
.png?width=869&height=597&name=image%20(5).png)
-1.png?width=486&height=315&name=IDC%20Banner%20(1)-1.png)
.png?width=300&height=175&name=Rectangle%2034624433%20(2).png)







.png?width=645&height=667&name=Widgets%20(2).png)













.png)




.webp)