Atlas Systems Named a Representative Vendor in 2025 Gartner® Market Guide for TPRM Technology Solutions → Read More

Best Provider and Physician Engagement Strategies


6 min read | Last Updated: 27 Jan, 2026
Medical providers not only deliver quality care, they also implement many of the system changes needed to improve care and operational efficiency. Getting their buy-in is vital for initiatives that increase access, quality, and value in the health care delivery system.
Engaging physicians goes beyond simply fulfilling clinical duties; it’s about improving outcomes, fostering teamwork, and driving positive change within the health systems.
This comprehensive guide explores physician engagement strategies in detail, offering practical tips to help you unlock the full potential of your healthcare team.
What is Provider Engagement?
Provider engagement refers to the strategies used to engage all healthcare providers, not just physicians (nurses, therapists, lab technicians, and more) to improve care quality and operational efficiency.
Why Provider and Physician Engagement Matters
When medical providers are supported and engaged, they provide better care, improving patient trust and loyalty. Here’s why provider and physician engagement matters:
Improved patient care
Provider engagement is crucial in healthcare organizations because it creates a collaborative environment that enhances the quality of patient care. Engaged providers are more invested in the care they deliver, which directly benefits patients. They communicate better with other staff, follow best practices, and make informed decisions, leading to higher-quality care.
Better care coordination
Engaged providers communicate more effectively with patients, healthcare staff, and care partners, creating a positive experience for all. Providers who feel valued and supported are more likely to raise concerns, share insights, and participate actively in discussions about patient care.
Improved organizational performance
When providers and care teams are aligned on organizational goals, they work hard to drive measurable improvements in care quality, patient safety, and cost control. They are more open to adopting new technologies and care models that help them deliver quality care.
Challenges to Physician Engagement
By understanding the unique issues that physicians face, your healthcare organization can create more effective, customized provider engagement strategies. Here are the top challenges to physician engagement:
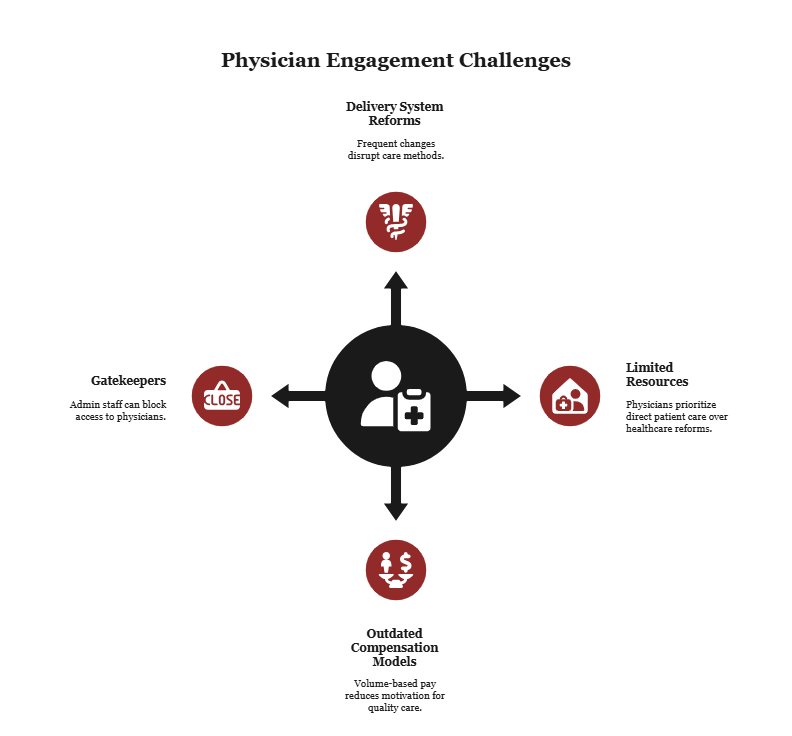
Regular delivery system reforms
Regular changes to the U.S. health care system can make it difficult for physicians to understand their role, how changes will impact them, and how to implement the latest regulations. They may consider new programs a threat to their traditional care delivery methods, fearing the loss of self-governance and revenue.
Physicians nearing the end of their careers may be less focused on long-term changes and more hesitant to adopt new technology. Additionally, these physicians typically rely on traditional service and payment models, which are often the focus of delivery system reform efforts.
Limited resources
Some physicians mistakenly think that health care reforms will increase their administrative burdens and reduce the time they dedicate to patients. They may also feel pressured to adopt new technologies or assign staff to reporting and care coordination without having clear evidence that these efforts will lead to better outcomes. When resources are limited, most physicians would rather devote their time and efforts to direct patient care.
Outdated compensation models
Many current compensation models fail to encourage physician engagement. They don’t reward participation in new care delivery models, collaboration, or quality outcomes. The pay structures still focus on patient volumes and services provided rather than quality of care.
They fail to recognize physicians’ efforts to improve care coordination and patient satisfaction. When medical providers feel their hard work goes unnoticed, their motivation and trust in the system decline. Align compensation with modern healthcare priorities to keep physicians committed to organizational goals.
Gatekeepers limit access to doctors
Administrative or front desk staff at physician offices often act as gatekeepers, preventing access to physicians. They can slow down or block efforts to engage physicians by delaying communication, prioritizing urgent clinical or administrative tasks, or preventing opportunities for direct interaction. Your provider engagement strategies should account for their role and involve them proactively.
Best Practices for Physician Engagement
These five strategies are designed for today’s healthcare environment and will help you reimagine how to support, motivate, and engage physicians.
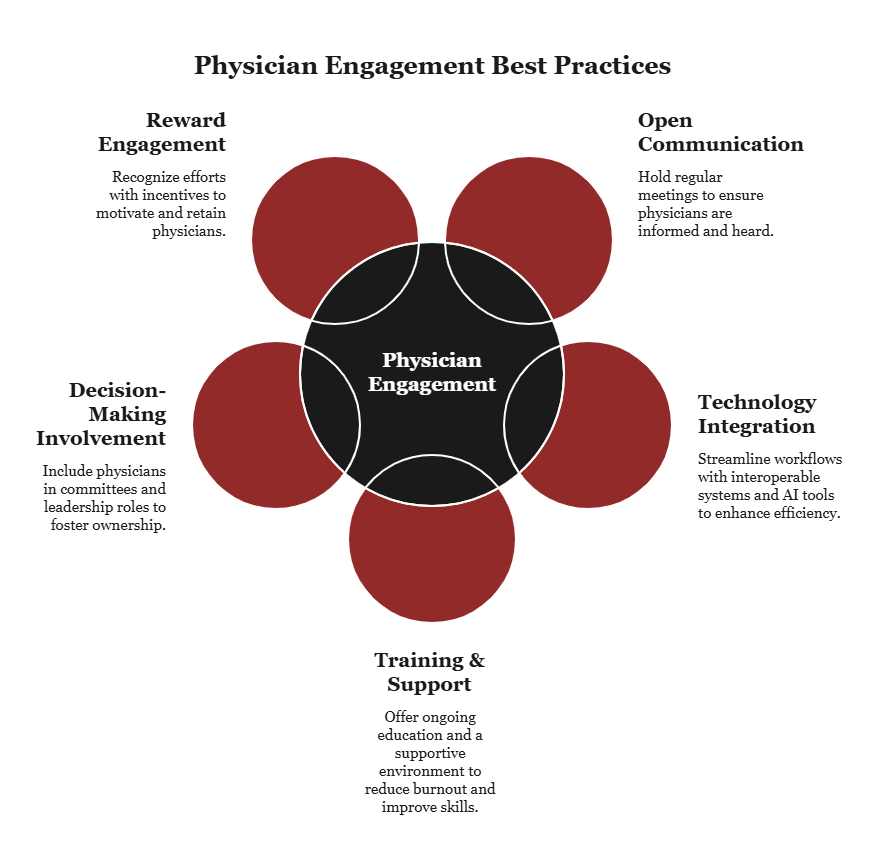
Create open communication channels
Open communication channels make physicians feel heard and valued, and they become more willing to contribute to organizational initiatives and improvements. Some ways to encourage open communication include having regular meetings where physicians can discuss clinical and administrative issues openly.
Your healthcare organization should also establish reliable feedback mechanisms to gather physicians' input on various issues. Be transparent about organizational changes and challenges to make physicians feel more invested in the organization’s success. Ensure leadership is accessible and approachable. This fosters trust and enhances provider engagement.
Use technology to simplify workflows
The efficiency of a physician’s workflow determines their engagement level. Cumbersome processes and outdated technology often lead to frustration and disengagement. Your healthcare facility should streamline and simplify workflows by having interoperable systems that allow information to flow seamlessly.
Provider engagement tools with AI and machine learning technologies can significantly simplify physicians’ workflows by streamlining routine tasks, improving data accuracy, and providing physicians with actionable insights. Data analysis tools can also help providers understand their performance and identify areas for improvement by providing real-time, actionable insights.
Train and support physicians
Offer physicians regular training and support to foster engagement. By continually upgrading their skills and knowledge, they can keep pace with the rapid advancements in healthcare. Offer both skill-based training and technology training to help them improve their clinical skills and use new medical technologies efficiently and effectively.
It’s also important to create a supportive work environment for physicians that reduces stress and prevents burnout. Support physicians in their continuing medical education to demonstrate your commitment to their professional growth.
Involve providers in decision-making
Physicians play a key role in every healthcare facility, and involving them in decision-making can greatly boost their engagement. Implement healthcare provider engagement strategies, such as adding providers to medical committees and boards, to enable their participation in discussions about the institution’s policies, procedures, and strategies. Involving them in critical decisions ensures that the decisions made are beneficial, practical, and likely to be well-received by the medical staff.
Include providers in strategic planning sessions so they can contribute to the institution’s long-term vision and direction. Also, appoint some as leaders so they can connect the administration and the medical staff.
Reward providers for engaging
Recognition and rewards significantly boost morale by making physicians feel valued and appreciated. They are more likely to be engaged and productive, and less likely to seek other practice opportunities. Regularly acknowledge physicians for their hard work and dedication in meetings, digital communication platforms, or through private feedback sessions. You can also offer financial incentives tied to their performance, such as bonuses for meeting specific quality or efficiency benchmarks.
Alternatively, you can offer incentives such as opportunities for professional development, like access to advanced training. Rewarding providers with initiatives that support work-life balance, like flexible scheduling, can enhance their job satisfaction and lead to higher engagement levels.
Make Your Provider Engagement Strategies Effective with PRIME® by Atlas Systems
Physician and provider engagement are key to the clinical and financial performance of healthcare organizations. When you get providers to embrace ownership, healthcare reforms become easier to implement.
Providers’ decisions often determine healthcare quality and cost outcomes, so it’s critical to have a shared vision that aligns their goals with those of the health system. Once you have their buy-in, you can implement quality improvement efforts that will benefit everyone.
Technology can make all the difference, enhancing provider engagement and ensuring they focus on what matters most: delivering quality care.
Our comprehensive provider lifecycle management platform, PRIME® improves provider engagement by streamlining administrative tasks, keeping provider data accurate, and promoting real-time collaboration between healthcare providers and health plans.
Boost provider engagement today with PRIME® by Atlas Systems: engage providers, enhance care, cut costs. Get a demo.
Frequently Asked Questions
1. What is the difference between provider engagement and physician engagement?
Provider engagement focuses on all healthcare providers, and the strategies used help improve care quality, patient satisfaction, and operational efficiency. Physician engagement, on the other hand, focuses specifically on doctors, and the strategies applied help increase their alignment with organizational goals, such as patient care quality and adherence to policies.
2. How do you measure physician engagement?
Physician engagement is measured through engagement surveys, retention and turnover rates, participation in projects and meetings, feedback and listening sessions, and performance and quality indicators such as patient satisfaction, adherence to care protocols, and fewer documentation errors.
3. What are examples of provider engagement strategies?
Examples of healthcare provider engagement strategies include involving providers in decision-making, improving communication, providing data and feedback on performance, offering financial incentives, and offering training and support. These strategies help healthcare organizations build stronger, more collaborative relationships with providers.
4. Why is provider engagement important in value-based care?
Provider engagement is crucial in value-based care, as providers make most decisions affecting patient outcomes and costs. The value-based care model rewards healthcare organizations for quality and efficiency, rather than volume, so it’s crucial to have engaged providers fully on board. They are more likely to follow best practices, which leads to better outcomes and lower costs. Without their commitment, it becomes much harder to succeed in a system that rewards value over volume.
.png?width=869&height=597&name=image%20(5).png)
-1.png?width=486&height=315&name=IDC%20Banner%20(1)-1.png)
.png?width=300&height=175&name=Rectangle%2034624433%20(2).png)







.png?width=645&height=667&name=Widgets%20(2).png)













.png)




.webp)